Technology + Healthcare Services: How does technology enhance the healthcare industry to enable better, more affordable, and more efficient healthcare?
To kick off our #Healthtech2019: “AI + Healthcare” conference, Dr. James Wall delivered a 40-minute keynote speech on technology and health services. As a practicing pediatric surgeon and the Director of Stanford Byers Center for Biodesign, Dr. Wall offered his perspectives on the impact of technological development on the traditional healthcare industry, as well as his outlook on the future of HealthTech. Despite Dr. Wall’s insistence on not being an expert in AI or robotics, we believe it is precisely because of this that he is able to provide an objective evaluation on AI and healthtech, based on a value-based driven approach.
Dr. Wall explained that there are many different visions on the application of AI in the healthcare field. There are notable influencers such as Deep Medicine author and Director of Scripps Research Translational Institute, Eric Topol, who propose that AI will become a sort of cognitive assistant for doctors, improving diagnostic efficiency while not replacing doctors. On the other hand, there are those who predict AI will wholly replace people in the medical system; everything, from diagnosis to surgery to pharmaceuticals, will be completed by machines.
The above viewpoints give insights into the current situation of the AI industry: “everybody talks about it, but nobody necessarily knows what they are doing with it. Everybody thinks everybody else is doing it in healthcare and thus claim they are doing it. Some people really are doing it, but they are not doing it right.” Dr. Wall mentioned during the conference.
Instead of immediately jumping into a discussion on AI and its application in healthcare, Dr. Wall started with a primer on the current situation in healthcare and HealthTech, before explaining what a value-based driven innovation approach looks like and examples of it.
Challenges Faced by the Healthcare Field and Targeted Solutions
Challenges Facing Healthcare:
Healthcare spending in the United States is exorbitant, a fact that is well-known and often lamented in the country. The US healthcare spending is twice as much as any other developed nation per patient. Despite annual medical expenses of more than $10,000 per person, US patients have not seen significant results or improvements.
Medical practitioners have a limited scope of experience. Even though there is a wealth of medical literature and practical experience opportunities (in the form of residencies), the amount of medical knowledge has been growing exponentially. In 1950, it took 30 years for the number of medical documents to double, but now, it only takes 70 days. Although not every piece of medical literature is worth reading, it is far beyond any individual’s ability to read everything and understand all the new developments.
The current payment incentives are not aligned with optimal outcomes. Payment is still done through a fee-for-service system. Almost all medical personnel are paid just for providing services, but not necessarily delivering the best outcomes.
Targeted Solutions:
Dr. Wall believes that technology is one of the greatest driving forces for promoting reforms in the healthcare system. With the integration of data, connectivity, and computing power, more efficient and more personalized healthcare can be enhanced. These, Dr. Wall stresses, must be coupled with value to deliver better outcomes at lower costs.
Another driving force for the reform of the healthcare system is the establishment of incentives to link medical payments to the quality of medical care. For example, there is Accountable Care Organizations, where hospital systems and healthcare systems take on the risk of an entire population with a fixed payment so that they're highly incentivized to keep them out of high cost environments like nursing facilities and hospitals. Another example is the bundled care within surgery. The medical institutions charge a fixed fee for patient procedures and the 90 days of care services afterwards. This model encourages medical institutions to provide patients with the best treatment at lower costs to reduce repeated visits, thus ensuring better care is provided from the start.
AI and Big Data: A Boon for Healthcare but with Challenges Ahead
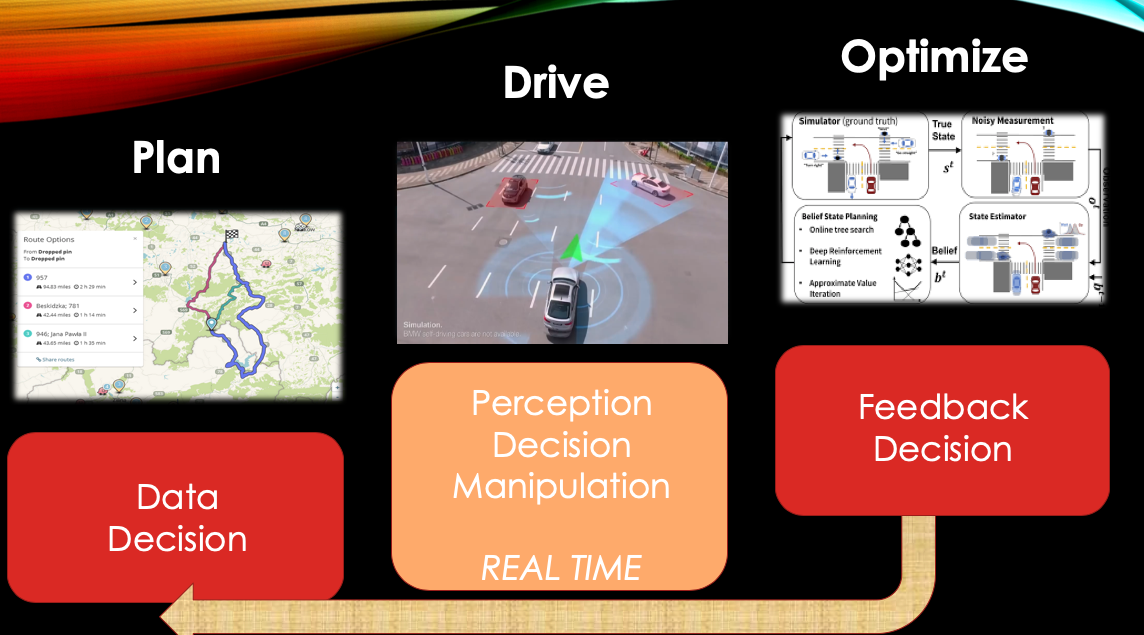
With the progress of healthtech, the traditional healthcare industry is entering a new era driven by data. The rise in the use of electronic health records facilitates the storage and analysis of patient data while the rise of wearable devices–such as the Apple Watch–enables users to track their health data in real time. Obtaining this data is a good start, but it is far from enough for medical purposes, as the data collected is largely diagnostic and does not require real-time analysis. Moreover, this so-called “big data” comes from already existing and highly structured data sets, which is a lot less messy than when people get into image processing, up to video processing, up to trying to integrate literature and other inputs.
Dr. Wall also indicated that government organizations, particularly the Food and Drug Administration (FDA), have not kept pace with the progress of technological development. The FDA has yet to list all FDA-approved medical technologies on its website; rather the current list of the eight FDA-approved medical technologies was compiled by Topol himself and shared on Twitter for reference. The FDA needs to update its digital health standards and guidance in a timely manner, so the information can be available to the public.
Should Healthtech Startups Take a Value Driven or Technology Driven Approach?
During our 2018 Forum on AI, Founder and CEO of Nightingale Security, Jack Wu, expressed that AI needs to understand and predict the needs of consumers and provide them with better, faster, and cheaper solutions, a view which Dr. Wall agrees. Nightingale Security, as a UAV security company, has a specific consumer base–mainly chief security officers. In comparison, the consumer base for healthcare companies includes medical institutions, doctors, patients, and the government. Each consumer segment has different needs and requirements for health technology, and this poses another challenge to anyone hoping to innovate in the healthcare field.
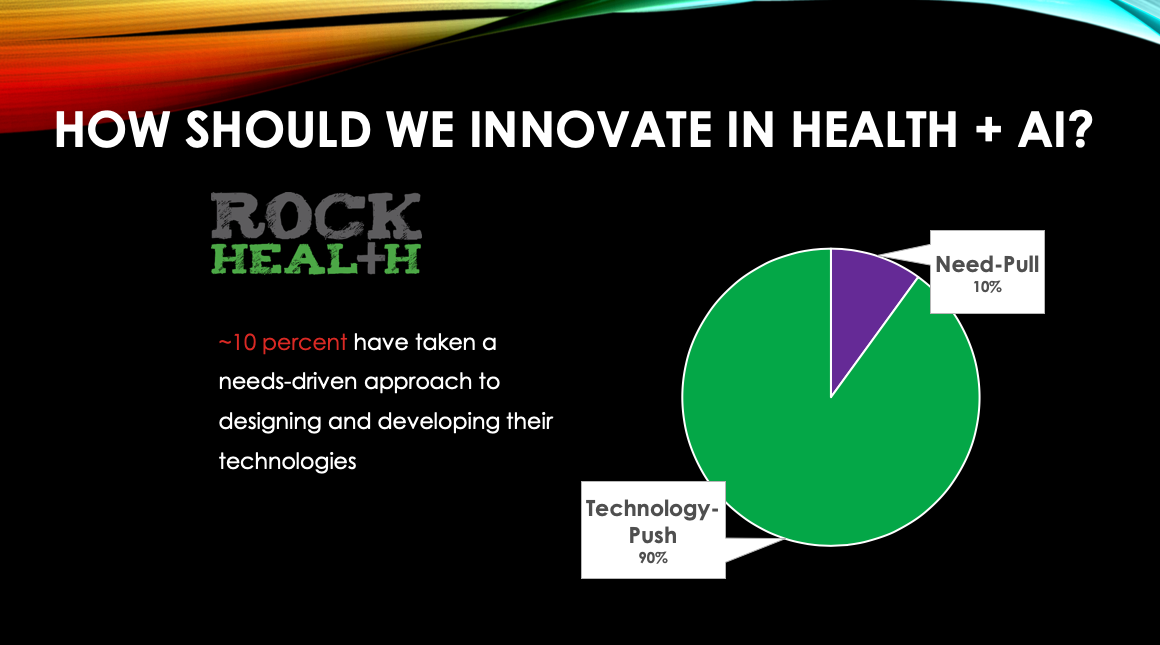
According to recent research reports from Rock Health, only about 10% of medical and health companies in the market are value-driven. These companies first observe the needs of patients, doctors, or hospitals before developing suitable technology, while the other 90% find suitable application scenarios for their developed technologies.
Technology-oriented companies may encounter various risks in the development process, because founders tend to overestimate the market size for and applications of their products. For example, one such company may think its product is suitable for all diabetic people, but in actuality, it might only be suitable for patients aged 15 to 20, with a hemoglobin AC of eight who stay at home. As a result, the market size shrinks immediately and the investment scale needs to be adjusted accordingly. Moreover, technology-first companies historically tend to avoid regulation, which usually means it does not want to commit to its medical products or services. This not only reduces the impact of the technology, but also results in not enough value being created to drive development in the healthcare industry.
How Should We Innovate in Healthcare?
Dr. Wall shared how Stanford Byers Center for Biodesign (Stanford Biodesign) innovates in healthcare. Established in 2000, Stanford Biodesign aims to create an ecosystem for Stanford University’s students, fellows, and faculty and provides support in the form of knowledge, skills, mentoring, and networking, so they can contribute meaningful medical innovations to patients around the world.
Resources
Stanford Biodesign funds diverse, multidisciplinary teams for one year and provides access to Stanford’s medical system, so they can observe current problems in the healthcare system and understand the opportunities for innovation.
Searching for pain points
During this time, a team is not meant to look for specific solutions, but to focus on searching for pain points: where patients are suffering, where hospitals are spending a lot of money, where providers are struggling, and more. Only by identifying pain points and understanding the problem can a team then come up with meaningful solutions, implement them commercially, and bring returns on investment. That’s why the teams at Stanford Biodesign usually spend around six months categorizing hundreds of problems into needs and conducting due diligence on them.
Innovation and Invention
Next, the team enters the invention phase, looking at services, AI technology, or mechanical equipment as solutions and examining the feasibility of such solutions by considering various factors like the IP landscape or the competitive landscape.
Dr. Wall believes the results of Stanford Biodesign speak for themselves. In the past 18 years, 55 startups have come out of Stanford Biodesign, 2 of which have gone public and some of which have been acquired. More importantly, 2.7 million patients have been treated by its technologies since its inception. Dr. Wall then reviewed three examples of the program–iRhythm, Tueo Health, and Radial Medical. They will not be described here, but if you are interested in the details, we invite you to read more about them on the Stanford Biodesign website.
The Future of Healthtech
Dr. Wall is full of hope for the application of AI in the field of healthcare, but he offers three points to which we should pay attention.
First, we have to ensure that our data sets are comprehensive: the data used for analysis should contain data from patients of all types, rather than a specific subset like white males in their 60s.
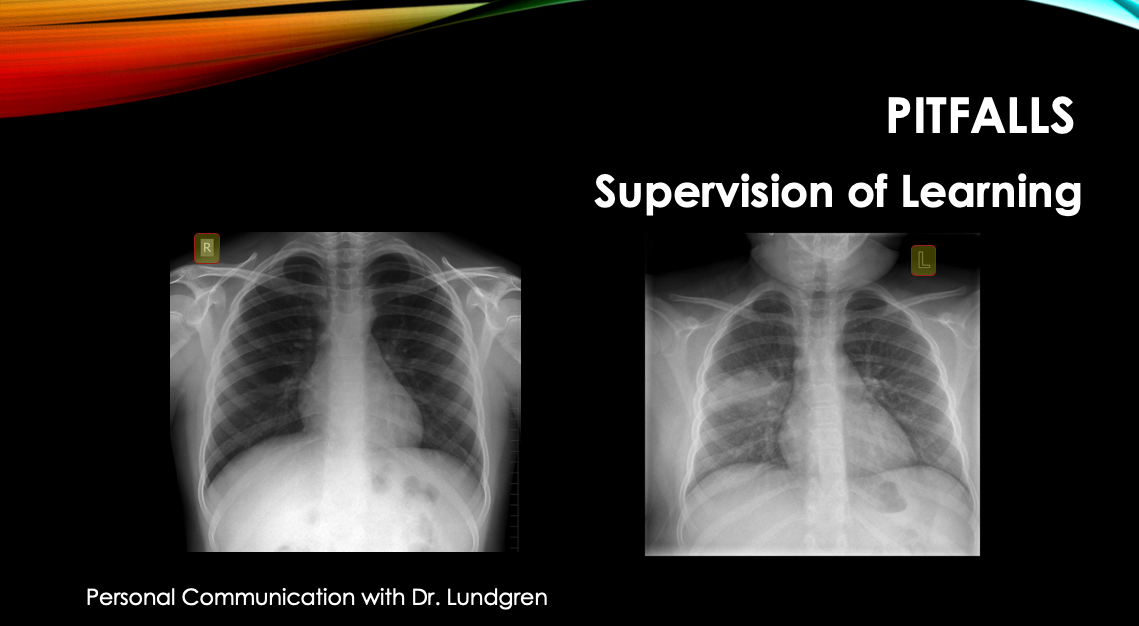
Second, we should verify that our algorithms are reasonable. For example, a medical team once obtained a large set of chest x-rays of pneumonia patients from one hospital and of normal patients from a different hospital. They put this data in an algorithm to have the computer identify pneumonia in the images. Although the computer successfully distinguished between the x-rays of normal people and pneumonia patients, the medical team later found that the algorithm classified the pictures mainly by comparing the different fonts used by the two hospitals, rather than analyzing the actual content of the images.
Third, we must pay attention to the risk of skill degradation. The rise of automation can bring convenience and efficiency to healthcare, but can also contribute to loss of skill in medical practitioners. For surgeons and physicians, this can be especially dangerous if issues arise. Ultimately, however, Dr. Wall hopes that AI and automation can develop to the point where it can offer cognitive assistance to practitioners, in order to complement their expertise and experience.
This year’s forum was full of lively dialogue and insightful discussions, many of which, unfortunately, cannot be conveyed here. We will continue publishing articles summarizing and analyzing topics from the forum, as well as reports from other relevant forums from time to time. If you are interested, we invite you to follow us on our social media.